蔡三军教授:结直肠癌腹膜转移诊治进展
一、背景
结直肠癌(colorectal cancer,CRC)是全球男性第三高发、女性第二高发的肿瘤[1]。结直肠癌腹膜转移(colorectal cancer peritoneal metastasis,CRCPM)是次于肝、肺转移的第三常见转移部位[2,3]。约5%的CRC患者会发生同时性腹膜转移(peritoneal metastasis,PM),约19%患者会发生异时性PM[4,5]。据报道88%的CRCPM通常伴有其他部位转移,常见于肝和肺[6]。PM患者如无积极有效治疗,通常生活质量差,生存时间短,且常并发腹痛、腹水和肠梗阻等症状[7-9]。
腹腔给药化疗是CRCPM重要的区域治疗手段,包括常温腹腔化疗、腹腔热灌注化疗((hyperthermicintraperitoneal chemotherapy,HIPEC)[10,11]以及近年来发展的加压腹腔内气溶胶化疗(Pressurized intraperitoneal aerosol chemotherapy,PIPAC)等[12]。外科腹膜减瘤术联合腹腔化疗以及全身治疗,使患者预后得以改善,生存质量得以提高[13]。
二、结直肠癌腹膜转移的诊断
(一)临床表现
结直肠癌腹膜转移在疾病初期往往并无明显临床症状,而随着疾病的不断演进和发展,在疾病晚期往往伴随严重的并发症表现。最常见的两大并发症表现为腹水和肠梗阻。相关研究表明,约28%~30%的患者在疾病晚期伴有腹水,而8%~20%的患者并发肠梗阻表现[2]。
(二)影像学诊断
近年来,虽然结直肠癌腹膜转移影像学诊断开展了一些相关研究,然而,影像学检测手段在腹膜转移的诊断方面仍然有待提高。
1. 超声 腹盆腔超声能够发现腹腔积液,也能观察直径较大的腹膜转移癌的形态。然而,对于小的腹膜转移癌,超声检查的准确性较低,应用价值有限。
2. 计算机断层扫描(CT) CT是检查肿瘤腹膜转移使用最多的方法。腹膜肿瘤结节大小影响CT检查的灵敏度,对于大于5cm的腹膜病灶,其诊断的灵敏度为90%,而针对小于0.5cm的病灶其灵敏度将下降为25%[14]。建议采用多层螺旋增强CT技术,结合三维重建有助于对于腹膜转移癌的系统评估。
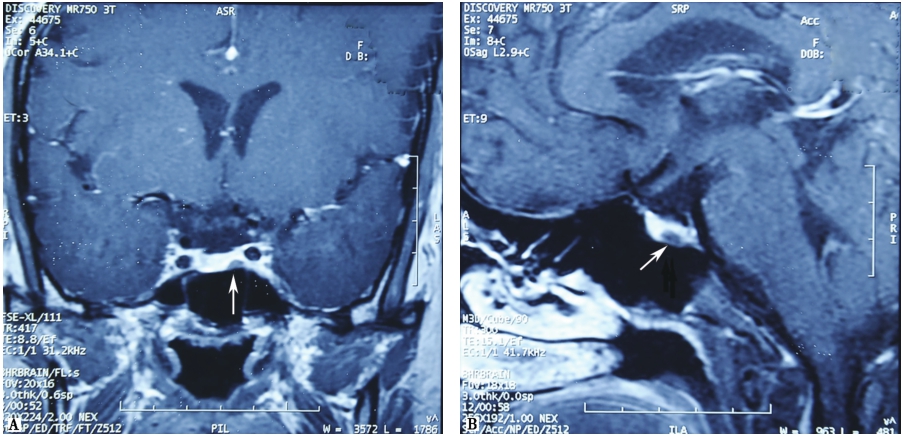
3. 磁共振成像(magnetic resonance imaging,MRI) 一项CT和MRI的对比研究显示,MRI诊断腹膜肿瘤的灵敏度高于CT[15]。Low等[16]报道,对于有中-大量腹水的患者,MRI可以评估被腹水覆盖的脏壁层腹膜病变情况,而CT则难于评估。研究发现,术前MRI评估结果与术中探查腹腔肿瘤严重程度、腹膜减瘤术彻底程度以及患者生存时间相关。说明MRI可作为选择适合腹膜肿瘤切除及HIPEC治疗的患者的评估手段之一[17]。复旦大学附属肿瘤医院的数据显示,全身弥散MRI在评估结直肠肿瘤腹膜转移方面有一定的价值,灵敏度、特异度和准确性分别为80.3%、84.5%和82.1%[18]。
4. 正电子发射计算机断层扫描(positron emission tomography,PET) 一项纳入了14项研究Meta分析指出PET/CT对腹膜转移肿瘤的诊断灵敏度和特异度较好,分别为87%(95%CI,77%~93%),92%(95%CI,89%~94%)[19]。近期的研究发现,PET可作为结直肠癌腹膜转移新辅助化疗反应情况的评估工具[20]。
三、结直肠癌腹膜转移的治疗
(一)肿瘤减灭术(Cytoreductive surgery,CRS)
与传统的姑息性手术不同,CRS治疗更加积极。腹膜转移瘤的手术经常需要切除腹膜转移灶及其累及的脏器组织,包括大网膜、小网膜、胆囊、阑尾和卵巢,甚至需合并切除部分小肠、直乙结肠、子宫、肝包膜、脾脏和远侧胃等脏器组织。尽管CRS手术范围较广泛,但是多数患者生活质量在术后6个月可恢复至基线水平[21,22]。减灭术完全性(completeness of cytoreduction,CCR)反应腹膜肿瘤减灭的彻底程度。评分分为:CCR-0:镜下无残留,CCR-1:任何一区域的残余肿瘤≤2.5mm,CCR-2:残余肿瘤>2.5mm且≤25mm,CCR-3:残余肿瘤>25mm[23]。CCR是重要的预后影响因素。一项法国的多中心临床研究纳入1990—2007年523例手术患者,结果显示完全性CRS患者的预后显著好于不完全性CRS患者的预后[24]。另一项系统综述结果表明,接受完全性CRS+HIPEC患者的中位生存期显著长于未接受完全性CRS的患者(33个月vs 12.5个月,P<0.05)[25]。
腹膜癌指数(peritoneal carcinomatosis index,PCI)是目前应用于评价腹膜肿瘤腹膜累及范围和严重程度最常用的分期系统[23,26]。PCI指数被众多学者认为是可用于筛选适合接受CRS手术的有效指标。研究显示,PCI>20的患者的中位生存时间明显短于PCI<20的患者(16个月vs 41个月,P=0.004)。多数学者认为,PCI>20是施行CRS手术的相对禁忌证[27,28]。
同时合并腹膜转移和肝转移的结直肠癌患者是否应该接受腹膜转移和肝转移灶的联合切除备受争议。有研究报道,联合治疗局限性腹膜转移和肝转移小于等于3处病灶的患者是可行且有益的[29-31],也有研究报道,腹膜转移伴肝转移患者进行CRS+HIPEC治疗的预后与单纯腹膜转移患者CRS+HIPEC治疗预后的差异不显著,腹膜转移伴肝转移和只有腹膜转移患者的中位总体生存分别为36个月(20~133个月)和25个月(14~82个月),P>0.05[32,33]。
(二)腹腔化疗
腹腔化疗可以是通过液体介质或气体介质。液体介质腹腔化疗是最常用的方法,按照温度可以分为常温腹腔化疗和加热腹腔化疗。加热腹腔化疗可以是灌注液加热后直接灌注化疗、腹腔灌注液内生场持续加热灌注化疗、微波加热持续升温腹腔灌注化疗和高精度持续循环热灌注化疗等。
术中或术后早期的腹腔化疗能让化疗药物在术后粘连形成及肿瘤细胞长入疤痕之前在腹腔内最大限度分布[34]。轻度高温(41~43℃)可通过多种机制发挥细胞毒作用,如DNA修复缺陷,蛋白变性,有氧代谢抑制等。此外,还可增强化疗药物的效果,以及促进药物进入肿瘤组织[35,36]。
腹膜转移曾被认为是恶性肿瘤终末期的表现,因此采取姑息性治疗[37],中位生存期仅6个月左右[2]。自从Sugarbaker教授提出腹膜肿瘤减灭术联合腹腔热灌注化疗(CRS+HIPEC),腹膜转移患者的生存得到明显改善[11]。研究发现,CRS+HIPEC可显著延长结直肠癌腹膜转移患者的生存时间,中位生存期达32~45个月,一些患者中位生存期可达63个月[13],且术后并发症率和死亡率并不算高[24,38,39]。
术后早期腹腔化疗(Early postoperative intraperitoneal chemotherapy,EPIC)通过腹部导管常温给药,并持续1~5天[10]。一项对比研究发现,HIPEC治疗组和EPIC治疗组,并发症发生率没有显著差异,分别为37%和19%(P>0.05),但中位总体生存时间分别为36.5个月和23.9个月(P=0.01),HIPEC组显著优于常温EPIC治疗[40]。
加压腹腔内气溶胶化疗(PIPAC)是近年来提出的治疗晚期腹膜转移的一种新的治疗方法,可通过腹腔镜给药,其优点有微创、低并发症、高生活质量、肿瘤内部药物浓度高、全身毒性反应少、药物分布和渗透效果好等[12,41,42]。研究发现,PIPAC局部药物浓度高,使用10%的常规化疗剂量即可使化疗耐药的腹膜转移病灶缩小[42]。Martin等[43]发表的前瞻性研究发现,PIPAC治疗后,67%患者腹膜肿瘤评分降低,23%患者腹水癌细胞阳性转阴性。一项纳入29篇PIPAC治疗腹膜转移的系统综述通过综合分析认为,PIPAC是可行、安全、耐受性好的治疗方式,初步显示具有良好的反应率[44]。
(三)全身化疗(Systemic chemotherapy,SC)
哪种全身治疗方案对于CRCPM目前没有定论。有研究显示,一线使用化疗联合贝伐单抗比单纯化疗有更大的生存获益[45]。CRS术前全身化疗可能使腹膜转移癌患者获益,约10%可达到病理完全缓解[46]。研究发现,CRS-HIPEC治疗后进行全身化疗的患者预后优于无全身化疗者[47]。
目前的共识认为,积极的全身治疗联合靶向治疗能够改善腹膜转移癌患者的预后;术后辅助全身治疗可能具有生存获益;对于高危复发人群,术前全身化疗联合CRS+HIPEC可能是优选策略。
四、结直肠癌腹膜转移的预后
与总体转移性结直肠癌患者预后相比,CRCPM患者的整体生存率较低。至今,CRCPM仍被认为是结直肠癌疾病进展的终末期[13],最新版的AJCC分期把腹膜转移单列为ⅣC期。
Franko等[8]通过对14项总共纳入了10553例接受全身化疗患者的前瞻性随机试验研究分析发现,9178(87%)例患者有非腹膜转移性结直肠癌,194(2%)例患者有孤立性CRCPM,1181(11%)例患者有CRCPM合并其他脏器转移。预后分析发现,孤立性非腹膜转移患者预后显著优于孤立性腹膜转移患者(孤立性肝转移患者HR 0.79,孤立性肺转移患者HR 0.61)。
来自荷兰的一项研究也报道了类似的结果[48],在CAIRO的研究中,CRCPM患者的中位生存时间为10.4个月,而非CRCPM的患者为17.3个月。而在CAIRO2的研究中,两者的中位生存时间为15.2个月和20.7个月(P<0.001)。
在全身化疗的基础上,CRS联合HIPEC的积极治疗能够改善CRCPM患者的预后。荷兰的一项RCT研究显示,CRS+HIPEC联合全身化疗比单纯的全身化疗组的中位生存时间延长9.7个月[49],在部分达到完全减瘤术的患者中,5年总生存率达到45%[39]。法国Gustave Roussy医院的报道也显示,CRCPM患者接受积极的CRS+HIPEC联合全身化疗者,5年总生存率达到36.5%,接近肝转移癌的治疗水平[50]。
五、结论
随着科学技术和研究的进步,CRCPM的诊断和治疗方面都取得了相应的进展。超声、CT、MRI和PET/CT在CRCPM的诊断评估方面各有优势和局限性,综合各种评估手段可能更加准确地评估腹膜转移癌。在CRCPM的治疗方面,治疗方法从以前的姑息性化疗发展到CRS联合腹腔化疗(EPIC、HIPEC、PIPAC)以及全身化疗的多学科综合治疗模式,患者预后和生活质量得到了提高。
参考文献
[1] Torre LA,Bray F,Siegel RL,et al. Global cancer statistics,2012. CA Cancer J Clin,2015,65(2):87-108.
[2] Jayne DG,Fook S,Loi C,et al. Peritoneal carcinomatosis from colorectal cancer. Br J Surg,2002,89:1545-1550.
[3] Tsikitis VL,Malireddy K,Green EA,et al. Postoperative surveillance recommendations for early stage colon cancer based on results from the clinical outcomes of surgical therapy trial. J ClinOncol,2009,27(22):3671-3676.
[4] Watanabe T,Itabashi M,Shimada Y,et al. Japanese Society for Cancer of the Colon and Rectum(JSCCR) guidelines 2010 for the treatment of colorectal cancer. Int J ClinOncol,2012,17 (1):1-29.
[5] van Gestel YR,de Hingh IH,van Herk-Sukel MP,et al. Patterns of metachronous metastases afer curative treatment of colorectal cancer. Cancer Epidemiology,2014,38(4):448-454.
[6] Franko J,Shi Q,Goldman CD. Treatment of colorectal peritoneal carcinomatosis with systemic chemotherapy:a pooled analysis of north central cancer treatment group phase Ⅲ trials N9741 and N9841. Journal of Clinical Oncology,2012,30(3):263-267.
[7] Coccolini F,Gheza F LM. Peritoneal carcinomatosis. World J Gastroenterol,2013;19):6979-6994.
[8] Franko J,Shi Q,JP M. Prognosis of patients with peritoneal metastatic colorectal cancer given systemic therapy:an analysis of individual patient data from prospective randomised trials from the Analysis and Research in Cancers of the Digestive System(ARCAD)database. Lancet Oncol,2016,17:1709-1719.
[9] Sadeghi B,Arvieux C,O G. Peritoneal carcinomatosis from non-gynecologic malignancies:results of the EVOCAPE 1 multicentric prospective study. Cancer,2000,88:358-363.
[10] Elias D,Blot F,El Otmany A,et al. Curative treatment of peritoneal carcinomatosis arising from colorectal cancer by complete resection and intraperitoneal chemotherapy. cancer,2001,92:71-76.
[11] Sugarbaker PH. Surgical Management of Carcinomatosis from Colorectal Cancer. Clin Colon Rectal Surg,2005,18(3):190-203.
[12] Odendahl K,Solass W,Demtroder C,et al. Quality of life of patients with end-stage peritoneal metastasis treated with Pressurized IntraPeritoneal Aerosol Chemotherapy(PIPAC). Eur J SurgOncol,2015,41(10):1379-1385.
[13] Elias D,Lefevre JH,Chevalier J,et al. Complete cytoreductive surgery plus intraperitonealchemohyperthermia with oxaliplatin for peritoneal carcinomatosis of colorectal origin. J ClinOncol,2009,27(5):681-685.
[14] Archer A,Sugarbaker PH,JS J. Radiology of peritoneal carcinomatosis. Cancer Treat Res,1996,82:263-288.
[15] RN L. Extrahepatic abdominal imaging in patients with malig-nancy:comparison of MR imaging and helical CT in 164 Patients. J MagnReson Imaging,2000,12:269-277.
[16] RN L. Magnetic resonance imaging in the oncology patient:evaluation of the extrahepatic abdomen. Semin Ultrasound CT MR,2005,26:224 -236.
[17] Klumpp B,Aschoff P,Schwenzer N,et al. Correlation of preoperative magnetic resonance imaging of peritoneal carcinomatosis and clinical outcome after peritonectomy and HIPEC after 3 years of follow-up:preliminary results. Cancer Imaging,2013,13(4):540-547.
[18] Zhang H,Dai W,Fu C,et al. Diagnostic value of whole-body MRI with diffusion-weighted sequence for detection of peritoneal metastases in colorectal malignancy. Cancer Biol Med,2018,15(2):165-170.
[19] SeOnG-JAnGKiM,Lee S-w. Diagnostic accuracy of 18F-FDG PET/CT for detection of peritoneal carcinomatosis;a systematic review andmeta-analysis. Br J Radiol,2017;90:20170519.
[20] Liberale G,Lecocq C,Garcia C,et al. Accuracy of FDG-PET/CT in Colorectal Peritoneal Carcinomatosis:Potential Tool for Evaluation of Chemotherapeutic Response. Anticancer Res,2017;37(2):929-934.
[21] Chia CS,Tan GHC,Lim C,et al. Prospective Quality of Life Study for Colorectal Cancer Patients with Peritoneal Carcinomatosis Undergoing Cytoreductive Surgery and HyperthermicIntraperitoneal Chemotherapy. Annals of Surgical Oncology,2016;23(9):2905-2913.
[22] McQuellon RP,Loggie BW,Fleming RA,et al. Quality of life after intraperitonealhyperthermic chemotherapy(IPHC) for peritoneal carcinomatosis. Eur J SurgOncol,2001;27(1):65-73.
[23] P J,PH. S. Current methodologies for clinical assessment of patients with peritoneal carcinomatosis. J ExpClin Cancer Res. 1996;15):49-58.
[24] Elias D,Gilly F,Boutitie F,et al. Peritoneal colorectal carcinomatosis treated with surgery and perioperative intraperitoneal chemotherapy:retrospective analysis of 523 patients from a multicentric French study. J ClinOncol,2010;28(1):63-68.
[25] Chua TC,Esquivel J,Pelz JO,Morris DL. Summary of current therapeutic options for peritoneal metastases from colorectal cancer. J SurgOncol,2013;107(6):566-573.
[26] Arjona-Sanchez A,Medina-Fernandez FJ,Munoz-Casares FC,et al. Peritoneal metastases of colorectal origin treated by cytoreduction and HIPEC:An overview. World J GastrointestOncol,2014;6(10):407-412.
[27] Esquivel J,Sticca R,Sugarbaker P,et al. Cytoreductive surgery and hyperthermicintraperitoneal chemotherapy in the management of peritoneal surface malignancies of colonic origin:a consensus statement. Society of Surgical Oncology. Ann SurgOncol,2007;14(1):128-133.
[28] Li Y,Zhou YF,Liang H,et al. Chinese expert consensus on cytoreductive surgery and hyperthermicintraperitoneal chemotherapy for peritoneal malignancies. World J Gastroenterol,2016;22(30):6906-6916.
[29] Carmignani CP,Ortega-Perez G,Sugarbaker PH. The management of synchronous peritoneal carcinomatosis and hemato-genous metastasis from colorectal cancer. Eur J SurgOncol,2004;30(4):391-398.
[30] Chua TC,Yan TD,Zhao J,Morris DL. Peritoneal carcinomatosisand liver metastases from colorectal cancer treated with cytor-eductive surgery perioperative intraperitoneal chemotherapy and liver resection. Eur J SurgOncol,2009;35(12):1299-1305.
[31] Elias D,Benizri E,Pocard M,et al. Treatment of synchronous peritoneal carcinomatosis and liver metastases from colorectal cancer. Eur J SurgOncol,2006;32(6):632-636.
[32] Varban O,Levine EA,Stewart JH,et al. Outcomes associated with cytoreductive surgery and intraperitonealhyperthermic chemotherapy in colorectal cancer patients with peritoneal surface disease and hepatic metastases. Cancer,2009;115(15):3427-3436.
[33] Lorimier G,Linot B,Paillocher N,et al. Curative cytored-uctive surgery followed by hyperthermicintraperitoneal chemotherapy in patients with peritoneal carcinomatosis and synchronous resectable liver metastases arising from colorectal cancer. Eur J SurgOncol,2017;43(1):150-158.
[34] Van der Speeten K,Stuart OA,Sugarbaker PH. Pharmacology of perioperative intraperitoneal and intravenous chemotherapy in patients with peritoneal surface malignancy. SurgOncolClin N Am,2012;21(4):577-597.
[35] Kusamura S,Dominique E,Baratti D,et al. Drugs,carrier solutions and temperature in hyperthermicintraperitoneal chemotherapy. J SurgOncol,2008;98(4):247-252.
[36] Sticca RP,BW. D. Rationale for hyperthermia with intraperit-neal intraoperative chemotherapy agents. SurgOncolClin N Am,2005;12):689-700.
[37] Koppe MJ,Boerman OC,Oyen WJG,Bleichrodt RP. Peritoneal Carcinomatosis of Colorectal Origin. Annals of Surgery,2006;243(2):212-222.
[38] Glehen O,Kwiatkowski F,Sugarbaker PH,et al. Cytoreductive Surgery Combined With Perioperative IntraperitonealChemoth-erapy for the Management of Peritoneal Carcinomatosis From Colorectal Cancer:A Multi-Institutional Study. Journal of Clinical Oncology,2004;22(16):3284-3292.
[39] Verwaal VJ,Bruin S,Boot H,van Slooten G,van Tinteren H. 8-year follow-up of randomized trial:cytoreduction and hyperthermicintraperitoneal chemotherapy versus systemic chemotherapy in patients with peritoneal carcinomatosis of colorectal cancer. Ann SurgOncol,2008;15(9):2426-2432.
[40] Cashin PH,Graf W,Nygren P,Mahteme H. Intraoperativehyperthermic versus postoperative normothermicintraperitoneal chemotherapy for colonic peritoneal carcinomatosis:a case-control study. Ann Oncol,2012;23(3):647-652.
[41] Solass W,Hetzel A,Nadiradze G,et al. Description of a novel approach for intraperitoneal drug delivery and the related device. SurgEndosc,2012;26(7):1849-1855.
[42] Solass W,Kerb R,Murdter T,Giger-Pabst U,Strumberg D,Tempfer C,et al. Intraperitoneal chemotherapy of peritoneal carcinomatosis using pressurized aerosol as an alternative to liquid solution:first evidence for efficacy. Ann SurgOncol,2014;21(2):553-559.
[43] Graversen M,Detlefsen S,Bjerregaard JK,Fristrup CW,Pfeiffer P,Mortensen MB. Prospective,single-center implementation and response evaluation of pressurized intraperitoneal aerosol chemotherapy(PIPAC) for peritoneal metastasis. TherAdv Med Oncol,2018;10(1758835918777036).
[44] Grass F,Vuagniaux A,Teixeira-Farinha H,Lehmann K,Demartines N,Hubner M. Systematic review of pressurized intraperitoneal aerosol chemotherapy for the treatment of advanced peritoneal carcinomatosis. Br J Surg,2017;104(6):669-678.
[45] Klaver YL,Leenders BJ,Creemers GJ,Rutten HJ,Verwaal VJ,Lemmens VE,et al. Addition of biological therapies to palliative chemotherapy prolongs survival in patients with peritoneal carcinomatosis of colorectal origin. Am J ClinOncol,2013;36(2):157-161.
[46] Passot G,You B,Boschetti G,et al. Pathological response to neoadjuvant chemotherapy:a new prognosis tool for the curative management of peritoneal colorectal carcinomatosis. Ann SurgOncol,2014;21(8):2608-2614.
[47] Kuijpers AM,Mehta AM,Boot H,et al. Perioperative systemic chemotherapy in peritoneal carcinomatosis of lymph node positive colorectal cancer treated with cytoreductive surgery and hyperthermicintraperitoneal chemotherapy. Ann Oncol,2014;25(4):864-869.
[48] Klaver YL,Simkens LH,Lemmens VE,et al. Outcomes of colorectal cancer patients with peritoneal carcinomatosis treated with chemotherapy with and without targeted therapy. Eur J SurgOncol,2012;38(7):617-623.
[49] Verwaal VJ,van Ruth S,de Bree E,et al. Randomized trial of cytoreduction and hyperthermicintraperitoneal chemotherapy versus systemic chemotherapy and palliative surgery in patients with peritoneal carcinomatosis of colorectal cancer. Journal of Clinical Oncology,2003;0(21):3737-3743.
[50] Elias D,Faron M,Iuga BS,et al. Prognostic similarities and differences in optimally resected liver metastases and peritoneal metastases from colorectal cancers. Ann Surg,2015;261(1):157-163.
蔡三军
教授,主任医师,博士生导师,复旦大学附属肿瘤医院大肠外科主任,大肠癌多综合治疗组首席专家,复旦大学大肠癌诊治中心主任。上海市疾病控制中心大肠癌专业委员会主任。上海市抗癌协会理事。中国抗癌协会大肠癌专委会前主任委员;上海市抗癌协会大肠癌专委会主委,中国临床肿瘤协作中心(CSCO)常委、继续教育委员会主任,CSCO科研基金学术委员会委员,中国CSCO肿瘤营养协会主任委员,中国疾病控制中心中国胃肠肿瘤管理项目副组长,中国老年学学会老年肿瘤专业委员会常委。美国临床肿瘤指南(NCCN)中国版专家委员会委员,NCCN大肠癌临床实践指南(中国版)外科执笔人,复旦-法国梅理埃联合实验室大肠癌项目负责人。担任The Chinese-German Journal of Clinical Oncology、《实用肿瘤杂志》《中国癌症杂志》《世界华人消化杂志》《抗癌》《中国肿瘤学年鉴》《临床肿瘤学杂志》《肿瘤研究与临床》等杂志编委及审稿专家。
来源:人民卫生出版社《临床知识》约稿
作者:蔡三军教授,复旦大学附属肿瘤医院大肠外科主任;莫少波,蔡国响
编辑:环球医学资讯丁好奇
- 评价此内容
- 我要打分
近期推荐
热门关键词
最新会议
- 2013循证医学和实效研究方法学研讨会
- 欧洲心脏病学会年会
- 世界帕金森病和相关疾病2013年会议
- 英国介入放射学学会2013年第25届年会
- 美国血液学会2013年年会
- 美国癫痫学会2013年第67届年会
- 肥胖学会 2013年年会
- 2013年第9届欧洲抗体会议
- 国际精神病学协会 2013年会议
- 妇科肿瘤2013年第18届大会
- 国际创伤压力研究学会2013年第29届…
- 2013年第4届亚太地区骨质疏松症会议
- 皮肤病协会国际2013年会议
- 世界糖尿病2013年大会
- 2013年国际成瘾性药年会
- 彭晓霞---诊断试验的Meta分析
- 武姗姗---累积Meta分析和TSA分析
- 孙凤---Network Meta分析
- 杨智荣---Cochrane综述实战经验分享
- 杨祖耀---疾病频率资料的Meta分析
合作伙伴
Copyright g-medon.com All Rights Reserved 环球医学资讯 未经授权请勿转载!
网络实名:环球医学:京ICP备08004413号-2
关于我们|
我们的服务|版权及责任声明|联系我们
互联网药品信息服务资格证书(京)-经营性-2017-0027
互联网医疗保健信息服务复核同意书 京卫计网审[2015]第0344号


 会员登录
会员登录

